Cartilage Injury
Cartilage Defects Of The Knee
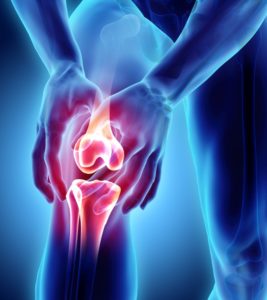
Cartilage defects of the knee involve damage to the articular cartilage, the smooth substance that covers the ends of the bones, keeping them from rubbing together. Cartilage defects may be degenerative, resulting from wear and tear, or traumatic, caused by an injury such as falling on the knee, jumping down, or rapidly changing directions while playing a sport. Such injuries do not always produce immediate symptoms because there are no nerves in cartilage. Over time, however, cartilage defects can disrupt normal joint function, leading to pain, inflammation, a grinding sensation in the knee and limited mobility.
Cartilage damage can range from a soft spot on the cartilage to a small tear in its top layer, to an extensive cartilage tear all the way to the bone. Such damage may gradually worsen or cause other problems in the joint. Since cartilage lacks a blood supply, the body cannot usually repair such defects on its own. Some severe tears that injure the bone, however, promote the growth of scar tissue known as fibrocartilage. This material while it replaces the missing articular cartilage, does not provide as smooth a gliding surface as the healthy cartilage, and so does not facilitate fluid motion.
Diagnosis Of Cartilage Defects
In order to diagnose a defect in the cartilage of the knee, the doctor will take a medical history and perform a physical examination. Imaging tests provide views of the tissue and bone within the knee to help the doctor evaluate the cause of the pain. The imaging tests performed may include X-rays, MRI and CT scans.
Treatment Of Cartilage Defects
Cartilage defects vary widely in size and degree. They need to be thoroughly assessed relative to location, severity, and the age and activity level of the patient, before a treatment plan can be determined. In most cases, surgery is necessary to provide relief from pain and increase mobility.
Debridement
Older patients who have smaller cartilage defects with mild symptoms may be suitable candidates for debridement. This arthroscopic procedure involves several small incisions into which a tiny camera and instruments are inserted. Loose or damaged tissue is removed, providing some relief, although typically the defects are not actually repaired during this procedure.
Microfracture
Microfracture is an arthroscopic procedure performed to repair damaged knee cartilage. During the microfracture procedure, a small surgical tool called an awl is inserted into the knee to create small holes, known as microfractures, in the bone near the defects. This process stimulates the release of cartilage-producing cells that will help to rebuild the damaged area.
Osteochondral Autograft Transplantation (OATS)
This procedure takes healthy cartilage from a non-weight-bearing area of the patient and transplants it to the site of the damage. This process is used for smaller defects, and involves filling the holes in the cartilage with small quantities of healthy transplanted tissue.
Autologous Chondrocyte Implantation
During this procedure, a sample of healthy cartilage is harvested, reproduced in large quantities outside the body, and then re-implanted onto the adjacent bone. This newly grown cartilage coats the bone, providing protection and support.
While surgery may be necessary, where there is only mild cartilage damage, conservative treatments, including resting the knee, wearing a brace, taking non-steroidal anti-inflammatory medications (NSAIDS), and getting injections of corticosteroids, may be sufficient to relieve symptoms.
Osteochondral Allograft Transplantation
Osteochondral allograft transplantation surgery (OATS) is a procedure that replaces damaged cartilage in the knee with healthy cartilage from a donor, relieving pain and restoring movement and function to the joint. Cartilage is the smooth coating on the end of the bones that provides cushioning and support for comfortable and fluid movement of the joints. Cartilage damage may occur as a result of injury or degeneration and can lead to severe pain and arthritis. Damaged cartilage can eventually wear away and leave the bone unprotected. Because damaged cartilage normally does not heal well on its own, several surgical techniques have been developed to stimulate the growth of new cartilage.
The OATS techniques involve transplanting healthy cartilage from from a cadaver to a damaged joint, to stimulate the growth of new cartilage in a damaged area. When cartilage has been restored through the OATS procedure, it can help to delay or prevent the onset of arthritis. The OATS procedure is ideal for patients with small areas of cartilage damage that can be easily repaired with a graft. Widespread cartilage damage cannot usually be treated with this procedure, since the graft may not provide enough material to completely rebuild the cartilage of the joint.
The OATS Procedure
During the OATS procedure, small plugs of healthy cartilage are taken from a cadaver donor and transferred to the area of damaged cartilage. Prior to the procedure, the donor cartilage is sterilized and prepared, and tested for any possible disease transmission. The OATS procedure is performed while the patient is sedated under general anesthesia. During the procedure, very small incisions are made over the affected joint and an arthroscope, a tiny instrument with a light and camera, is inserted. The surgeon examines the interior of the joint and removes any debris. Additional tiny incisions are made to introduce the plugs of donor cartilage into the joint. The surgeon uses tools to create openings in the damaged areas of cartilage to exactly fit these plugs, then grafts them into place. After they have been transplanted, the incisions are sutured closed.
Risks Of Osteochondral Allograft Transplantation
While the OATS procedure is considered a safe procedure, there are potential risks, which may include the failure of the donor cartilage to integrate completely with the patient’s existing cartilage. Additional complications may include:
- Infection
- Bleeding
- Joint stiffness
- Tissue damage
There is also a minimal chance of contracting an infection or disease from the donor tissue. Patients should consider these risks before deciding to have the OATS procedure.
Recovery From Osteochondral Allograft Transplantation
After the OATS procedure, the joint is bandaged. Swelling is common and regular applications of ice are recommended. Medication may also be prescribed to treat pain. Following the procedure, individuals may use a continuous passive motion (CPM) machine to keep the joint moving and to alleviate joint stiffness. Patients are typically advised to rest the affected joint for one to two weeks after the surgery. Most patients will use crutches for 6 to 12 weeks after surgery before they can successfully bear weight on the joint again. A physical therapy program helps to restore mobility and improve strength and flexibility of the affected joint. While recovery times vary, exercise and and regular activity can normally resume 2 to 3 months after the OATS procedure.