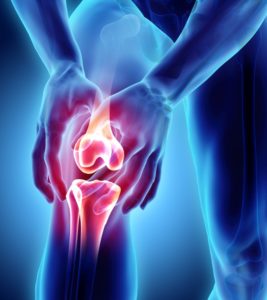
Dislocated Patella
Distal Realignment Of The Knee
Distal realignment procedures involve a repositioning of the structures of the kneecap. They are performed in order to correct patellofemoral instability, a chronic dislocation of the knee joint attaching the kneecap (patella) to the thigh bone (femur). There are several types of distal realignment surgeries, but they all involve shifting the tendon located beneath the kneecap to align it properly with the tibial tubercle, the bump on the shin bone of the lower leg found just below the knee.
Patellar instability is frequently the result of subluxation, a partial dislocation in the knee. It can cause symptoms including knee pain, a feeling that the kneecap is loose and a buckling of the knee. This area is where several tendons, ligaments and muscles are attached, so it is vulnerable to problems due to injury or because certain people are anatomically prone to the patella tracking slightly to one side.
Patellofemoral instability may in some cases be successfully treated with conservative measures that may include avoiding certain activities, performing exercises to strengthen the quadriceps muscle of the thigh and wearing a brace on the affected knee. However, in many patients, these methods do not provide significant relief of symptoms and a surgical procedure is necessary.
Types Of Distal Realignment Procedures
All types of distal realignment procedures are variations on the way in which the tendon and tibia tubercle are moved and altered within the knee. Although other procedures have been performed in the past, recent government studies have shown three surgical procedures to be most effective: the Elmslie-Trillat procedure, the Fulkerson procedure, and the Roux-Goldthwait procedure. Two procedures previously performed, the Maquet procedure and the Hauser procedure, have now fallen out of favor.
The Distal Realignment Procedure
While each type of distal realignment procedure varies slightly in how the surgeon treats the tendon and tibial tubercle, all are typically performed with the patient under general anesthesia. The surgery is usually completed in 60 to 90 minutes. Sometimes a distal realignment is performed as an outpatient procedure, but more often requires a hospital stay of 1 or 2 nights.
The surgeon will make an incision toward the lower front of the knee to gain access to the bone and tissue of the kneecap. The tibial tubercle is cut and moved slightly toward the inner side of the knee. The patellar tendon is then similarly relocated and realigned as necessary. The portion of the tibial tubercle that was cut is then reattached and secured using metal screws. Once all of the structures have been repositioned as needed, the surgeon can suture the incision.
Recovery From A Distal Realignment
Patients typically experience some pain after a distal realignment procedure and pain medication is prescribed. Swelling in the knee is common during the first few days after the operation, but this usually responds well to elevation of the knee and regular applications of ice.
The treated knee requires some level of support and protection to promote healing, so generally either a cast or a knee immobilizer is used. In addition, because the knee cannot safely bear full weight for some time, patients are required to use assistive devices such as crutches or canes for up to 6 weeks after the procedure. Physical therapy is an important part of the recovery process as it helps the knee to regain strength, flexibility and complete function.
Patients can often return to sedentary jobs after 3 or 4 days. However, more physical types of employment and other active pursuits generally cannot be resumed for at least 2 months following surgery.
Risks Of A Distal Realignment Procedure
While distal realignment procedures are considered safe and effective forms of surgery, all surgical procedures carry some risk. The risks associated with a distal realignment procedure may include infection, pain, prolonged healing of the bone and a decrease in range of motion in the knee.